| Structure | Name/CAS No. | Articles |
|---|---|---|
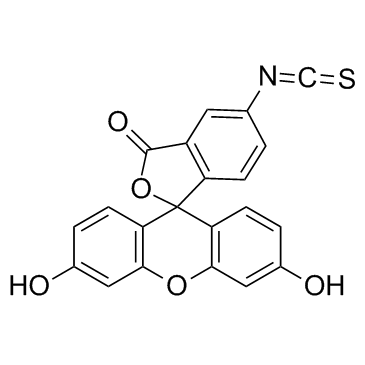 |
Fluorescein isothiocyanate
CAS:3326-32-7 |
|
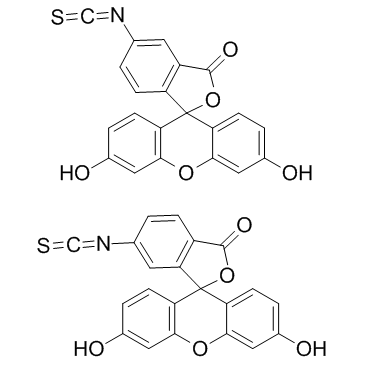 |
fluorescein 5-isothiocyanate
CAS:27072-45-3 |
|
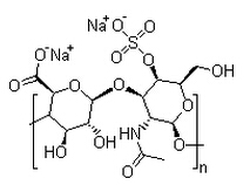 |
Chondroitin sulfate A sodium salt
CAS:39455-18-0 |
|
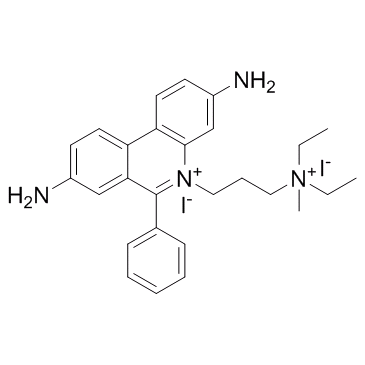 |
Propidium Iodide
CAS:25535-16-4 |