| Description |
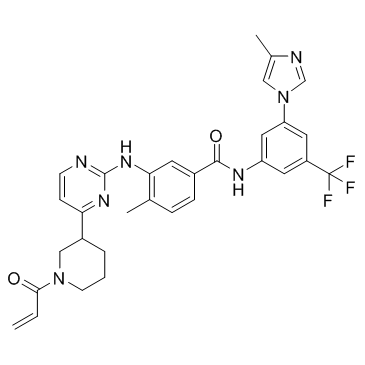
M443 is an irreversible and specific inhibitor of MRK, with an IC50<125 nM.
|
| Related Catalog |
|
| Target |
IC50: <125 nM (MRK)[1].
|
| In Vitro |
MRK depletion decreases cell viability after IR by 33% of control at 3 Gy. Similarly, the clonogenic assay shows a significant decrease in survival with a dose enhancement factor (DEF) of 1.6 at 10% viability. MRK activation by IR is maximal at 30 minutes after exposure to radiation. Therefore, for subsequent analysis, this time point is used. In both cell cultures, the IR-stimulated activation of MRK, Chk2, and p38 is greatly inhibited by 500 nM M443. Cells are seeded on coverslips, pretreated with 500 nM M443 or vehicle, exposed to 6 Gy of IR, fixed at different times after IR and processed for immunofluorescence with the MPM2 phospho-specific antibody that specifically stains mitotic cells. In contrast to control cells, the M443-treated cells fail to arrest after IR and maintained a similar mitotic index as the nonirradiated cells. Thus, inhibition of MRK leads to inhibition of Chk2 and failure to arrest in the cell cycle in response to IR-induced DNA damage[1].
|
| In Vivo |
Control mice survive with a median of 32 days after tumor cell implantation. Treatment with M443 alone adds 5.5 days to this survival, whereas the chosen low dose of radiation does not significantly increase survival. In contrast, the combination of M443 and IR extend survival with a median of 16 days longer than control. Treatment with M443 does not affect the animal weight, as the weight loss observed is observed in all groups just a few days before the animals became moribund. It is showed that the tumor-containing fraction has elevated levels of both total and active MRK (lane RB in the vehicle-treated brain). In contrast, the tumor-containing fraction from the M443-treated brain shows total loss of MRK activity. Interestingly, the fractions containing normal brain, which in the control brain show some level of MRK protein, in the treated brain also has lost MRK, suggesting that diffusion of M443 across the whole cerebellum inhibit normal MRK as well[1].
|
| Cell Assay |
Two days after transfection with siRNAs, medulloblastoma cells are seeded in a 96-well plate, and the following day, they are exposed to different doses of radiation. Cell viability is determined 72 hours after radiation treatment by MTT absorbance at 595 nm. For cells that are treated with M443 (250 nM, 500 nM), 6 hours after treatment with different concentrations of the drug or vehicle control, they are exposed to radiation and processed for the MTT assay 72 hours later as above. Five hundred cells are seeded in 6 cm dishes 2 days after siRNA transfections. The following day, cells are exposed to the different doses of radiation using a biologic irradiator and cultured for 7 days with media changes every other day. Colonies containing more than 50 cells are counted, and the results are used to calculate the surviving fractions. For the treatment with M443 or vehicle control, 24 hours after seeding, cells are exposed to the drug for 6 hours and subsequently to radiation[1].
|
| Animal Admin |
Mice[1] The primary UI226 medulloblastoma cells are patient derived xenografts. UI226 is largely propagated as flank cultures in nude mice and cultured in StemPro media for less than 3 weeks before intracranial injections. Medulloblastoma cells (5.0×105 UI226 in 5 mL of StemPro medium) are injected over 5 minutes into the cerebellum of 4-week-old athymic female mice. Three weeks after tumor cell implantation and approximately 2 weeks before the animals become moribund; treatment is started by implantation of an osmotic pump filled with either 0.05 mg/mL solution of M443 or vehicle (0.01% DMSO in PBS) and implanted in a subcutaneous pocket on the dorsal flank of the animal. A catheter with attached cannula delivers the drug intracranially and directly into the tumor over a period of 2 weeks, at a steady rate of 0.25 mL/hour. Irradiation of the mice head is initiated 2 days after pump implantation and conducted over 2 days[1].
|
| References |
[1]. Markowitz D, et al. Pharmacological Inhibition of the Protein Kinase MRK/ZAK Radiosensitizes Medulloblastoma. Mol Cancer Ther. 2016 Aug;15(8):1799-808.
|