Short-course oral co-trimoxazole versus intramuscular benzathine benzylpenicillin for impetigo in a highly endemic region: an open-label, randomised, controlled, non-inferiority trial.
Asha C Bowen, Steven Y C Tong, Ross M Andrews, Irene M O'Meara, Malcolm I McDonald, Mark D Chatfield, Bart J Currie, Jonathan R Carapetis
文献索引:Lancet 384(9960) , 2132-40, (2014)
全文:HTML全文
摘要
Impetigo affects more than 110 million children worldwide at any one time. The major burden of disease is in developing and tropical settings where topical antibiotics are impractical and lead to rapid emergence of antimicrobial resistance. Few trials of systemic antibiotics are available to guide management of extensive impetigo. As such, we aimed to compare short-course oral co-trimoxazole with standard treatment with intramuscular benzathine benzylpenicillin in children with impetigo in a highly endemic setting.In this randomised, controlled, non-inferiority trial, Indigenous Australian children aged 3 months to 13 years with purulent or crusted non-bullous impetigo were randomly assigned (1:1:1) to receive benzathine benzylpenicillin (weight-banded injection), twice-daily co-trimoxazole for 3 days (4 mg/kg plus 20 mg/kg per dose), or once-daily co-trimoxazole for 5 days (8 mg/kg plus 40 mg/kg per dose). At every visit, participants were randomised in blocks of six and 12, stratified by disease severity. Randomisation was done by research nurses and codes were in sealed, sequentially numbered, opaque envelopes. Independent reviewers masked to treatment allocation compared digital images of sores from days 0 and 7. The primary outcome was treatment success at day 7 in a modified intention-to-treat analysis. This trial is registered with the Australian New Zealand Clinical Trials Registry, number ACTRN12609000858291.Between Nov 26, 2009, and Nov 20, 2012, 508 patients were randomly assigned to receive benzathine benzylpenicillin (n=165 [156 analysed]), twice-daily co-trimoxazole for 3 days (n=175 [173 analysed]), or once-daily co-trimoxazole for 5 days (n=168 [161 analysed]). Treatment was successful in 133 (85%) children who received benzathine benzylpenicillin and 283 (85%) who received pooled co-trimoxazole (absolute difference 0·5%; 95% CI -6·2 to 7·3), showing non-inferiority of co-trimoxazole (10% margin). Results for twice-daily co-trimoxazole for 3 days and once-daily co-trimoxazole for 5 days were similar. Adverse events occurred in 54 participants, 49 (90%) of whom received benzathine benzylpenicillin.Short-course co-trimoxazole is a non-inferior, alternative treatment to benzathine benzylpenicillin for impetigo; it is palatable, pain-free, practical, and easily administered.Australian National Health and Medical Research Council.Copyright © 2014 Elsevier Ltd. All rights reserved.
相关化合物
| 结构式 | 名称/CAS号 | 分子式 | 全部文献 |
|---|---|---|---|
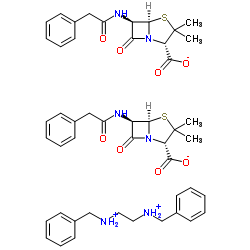 |
苄星青霉素
CAS:1538-09-6 |
C48H56N6O8S2 |
|
Treatment of late-stage syphilis--reply.
2015-03-03 [JAMA 313(9) , 969-70, (2015)] |
|
Treatment of late-stage syphilis.
2015-03-03 [JAMA 313(9) , 968-9, (2015)] |
|
Clinical features and incidence rates of ocular complication...
2015-02-01 [Am. J. Ophthalmol. 159(2) , 334-43.e1, (2015)] |
|
Treatment of impetigo in resource-limited settings.
2014-12-13 [Lancet 384(9960) , 2090-1, (2014)] |
|
Clavi syphilitici–an unusual presentation of syphilis
2014-06-01 [J. Am. Acad. Dermatol. 70(6) , e131-2, (2014)] |